Stroke In Children
What is a stroke?
A stroke is usually thought of as a condition that only affects adults. In fact, children can have them too.
While they are quite rare in childhood, some youngsters are more at risk than others. Around half of those who suffer a stroke will have an underlying medical condition. But the other half will have been apparently healthy beforehand. Strokes can affect many things including a child’s movement, speech, behaviour and learning. However, the good news is that in the majority of cases these effects are mild. It’s a good idea to be aware of strokes in childhood and what to look out for.
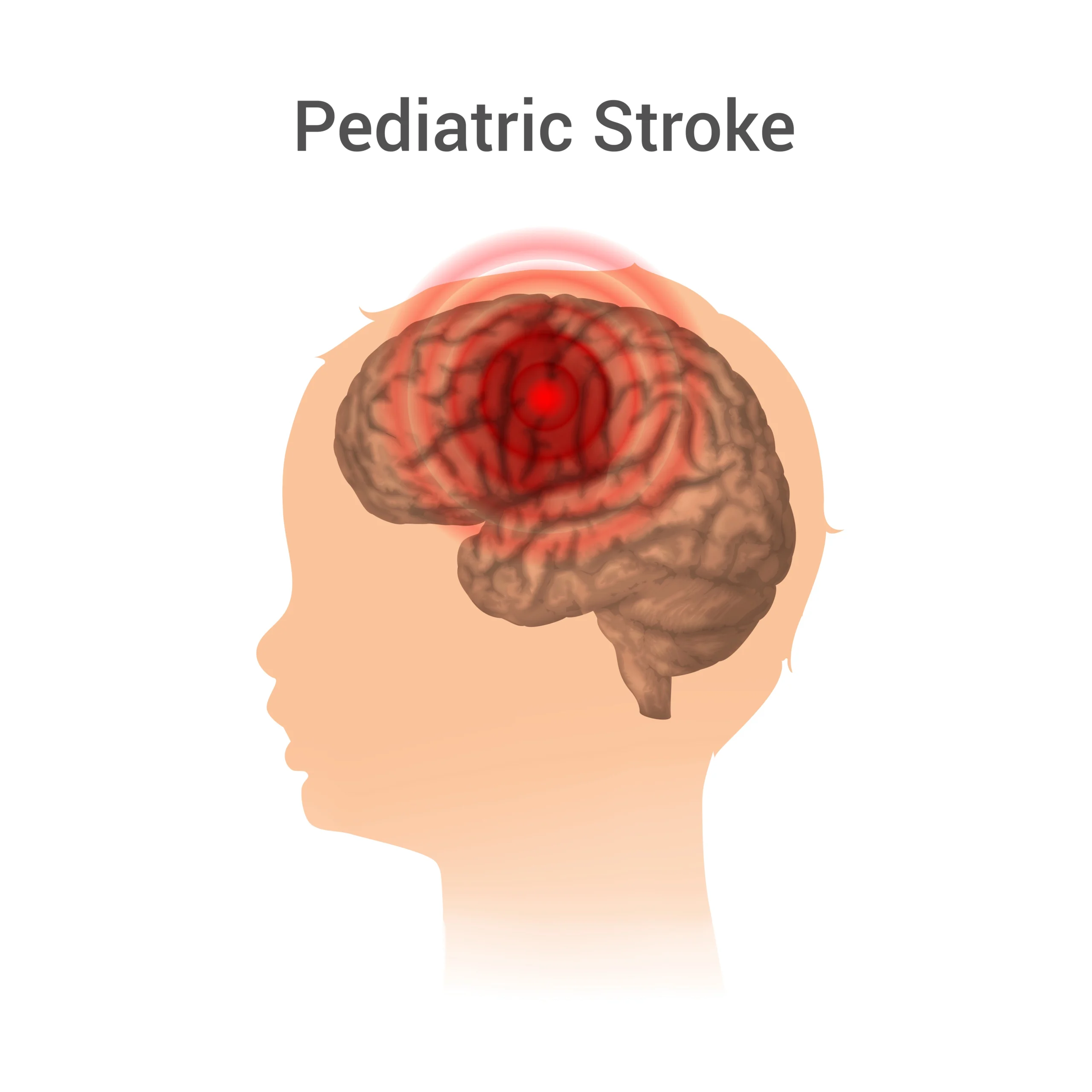
A stroke is a sudden disruption to the blood supply of the brain. It can affect some of the key functions that are controlled by the brain, such as movement and speech. The symptoms vary from child to child depending on the area of the brain that has been affected.
There are two main types. Both types can cause damage to brain cells:
- Ischaemic stroke – this happens when the blood supply to one area of the brain becomes blocked.
- Haemorrhagic stroke – this happens when blood leaks into brain tissue.
Why does this happen in childhood?
Children with an underlying medical problem, such as a heart condition or sickle cell anaemia , run a higher than usual risk of having a stroke. In some cases, a blood clotting problem (that can run in families) may be linked. But in children who don’t have an associated condition, there are lots of possible causes of stroke. One of the most common is a rare complication of chickenpox, which results in narrowing of the blood vessels in the head. Other causes include abnormalities affecting the blood vessels supplying the brain, which may then be vulnerable to the sort of minor head injury so common in children. In around ten per cent of children who have a stroke, no cause can be identified despite extensive tests.
What are the signs and symptoms?
Signs and symptoms vary depending on the area of the brain affected. In general, the most common effect is weakness down one side of the body. This can be difficult to detect in a young child – it may appear that your child has problems with balance. A child’s face can also droop on one side, and speech may be affected. An older child may complain of a headache at the time of a stroke.
How is it diagnosed?
Stroke is now recognized as a medical emergency. The signs of a stroke that can be recognised by family and friends, as well as professionals, are emphasized by the catchy word ‘FAST’.
FAST stands for:
- Facial weakness
- Arm (and leg weakness)
- Speech problems
- Time to dial Ambulance
Once your child has been diagnosed as having had a stroke, tests will be needed to try to establish a cause so that treatment can then be planned.
These tests may include:
- Magnetic resonance imaging (MRI) to identify the area of the brain affected.
- Blood tests to check for clotting problems or infection.
- An ‘echo’ scan to check your child’s heart
- A lumbar puncture to remove a tiny amount of cerebrospinal fluid (which surrounds the brain) to check for infection
- An angiogram, which gives detailed information about the blood vessels supplying the brain
What's the treatment?
No two children recover in exactly the same way after a stroke. Progress will depend on the area of the brain affected, and what caused the stroke in the first place. There are a number of different treatments depending on the needs of an individual child.
Medication can include aspirin, heparin or warfarin, which make the blood thinner and less likely to clot. Occasionally, children may be candidates for clot-busting drugs very soon after the stroke. For a child with underlying sickle cell anaemia, regular blood transfusions are used. If a child has a blood vessel blockage, surgery may be possible to try to improve the blood flow to the brain.
Rehabilitation team
All children will also need the help of a rehabilitation team including an occupational therapist, physiotherapist and/or speech and language therapist. This is the most important part of treatment.
The aim is to make a child’s daily activities easier, boost self-esteem and raise a child’s confidence. Therapy starts by assessing movement, play and independence skills, and you will be given ideas for home and school to develop your child’s skills and improve muscle tone and movement. The team may recommend and provide equipment, such as ankle or hand splints, to help your child move more easily and reduce the risk of permanent joint stiffness. The family is very important at this stage. The team will do everything they can to answer all your questions and to help you to support your child.
What's the outlook?
Improvements in many areas may continue to be seen for several months after the initial stroke. Our research has shown that all children recover the ability to walk independently after a stroke unless they have an additional illness or, very unusually, have had strokes on both sides of the body. Recovery in the affected arm, and in particular the hand, is usually the most significant movement problem. If their dominant hand is affected, some children adapt by using their other side for more tasks.
Speech and language problems improve most rapidly over the first year. The good news is that most children understand and speak normally after a stroke. Both language (if affected) and learning need to be formally assessed; Sometimes a child’s behaviour can be affected. This depends partly on the area of the brain affected but problems can include difficulties with attention and concentration. Your child will be monitored carefully in the months following the stroke and should make a good overall recovery in time.